The new eCQM for pressure injuries is here.
Are you ready to start reporting Stage 2 and Deep Tissue Pressure Injuries?
The CMS Hospital Harm – Pressure Injury (HH-PI) eCQM requires hospitals to report all new Stage 2 and Deep Tissue Pressure Injuries (in addition to Stage 3, 4, and Unstageable). While reporting for the eCQM is voluntary in CY 2025, it is scheduled to become MANDATORY in 2028.
WoundVision partners with hospitals across the country to transform pressure injury documentation and streamline surveillance with best in class EMR-integrated workflows, ensuring nothing falls through the cracks.
Check out the information below and access our HH-PI eCQM Calculator to see your estimated performance rate.

Important Facts
Don't overlook these critical components of the HH-PI eCQM.
Stage 2/DTPI Inclusion
This eCQM will require hospitals to report all new Stage 2-4, Unstageable and DTPIs.

Mandatory
The HH-PI measure is scheduled to become mandatory.
Lower is Better
A lower score reflects higher quality (the ideal score is 0%).
One PI Per Patient
For patients with multiple new pressure injuries, only one is counted.

Penalty
25% reduction in the market basket update if requirements not met.
RATIONALE
Pressure injuries (PIs) are a serious event and one of the most common patient harms. This safety eCQM captures the number of patients who experience harm in the form of a PI using direct extraction of structured data from the EHR to provide hospitals with reliable and timely measurement of their PI rates.
MEASURE DESCRIPTION
This eCQM assesses the proportion of inpatient hospitalizations for patients ages 18 years and older at the start of the encounter who suffer the harm of developing a new stage 2, stage 3, stage 4, deep tissue, or unstageable PI.
GOAL
By incentivizing hospitals to adopt best practices in PI prevention and treatment, CMS aims to enhance patient safety.
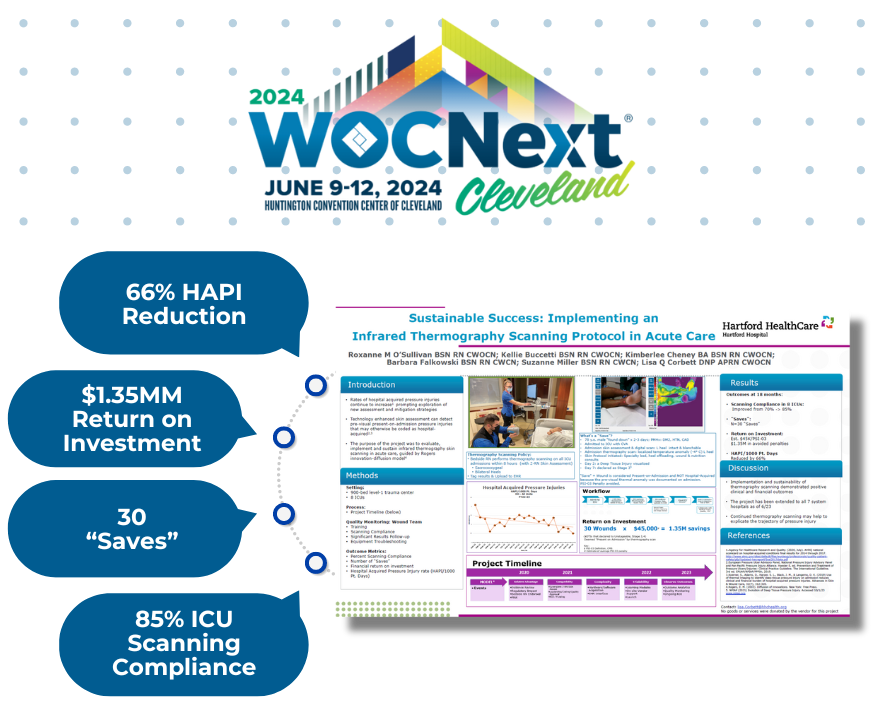
Transform Your Skin & Wound Assessment at WOCNext 2024
Rated as the "Highest Scoring Poster Abstract" at the 2023 SAWC Fall conference, Hartford Healthcare shares how they implemented skin temperature assessment across 7-hospital IDN.
Check out the full poster by filling out the form below.
How Does Measurement Work?
INITIAL POPULATION
All adult patients (age 18 or older) who were inpatient hospitalizations during the measurement period. This includes patients transitioning from the ED or observation to inpatient care within one hour.
A. DENOMINATOR
The denominator is equal to the initial population.
B. DENOMINATOR EXCLUSIONS
The denominator exclusions represent PIs that were outside of the hospital's control. This includes:
- Deep tissue pressure injury (DTPI) found on exam 72 hours or less after the admission
- Stage 2, 3, 4 or unstageable PI diagnosis present on admission (POA)
- Diagnosis of a COVID-19 infection during the admission
C. NUMERATOR INCLUSIONS
The numerator represents inpatient hospitalizations for patients with a new PI. This includes:
- Diagnosis of DTPI not POA or found on exam >72 hours after the admission
- Diagnosis of stage 2, 3, 4 or unstageable PI not POA or found on exam >24 hours after the admission
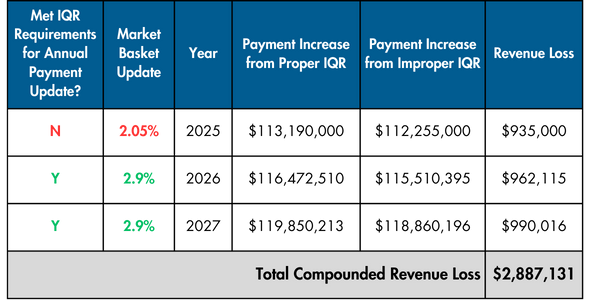
25% Penalty For Improper IQR
The Hospital Inpatient Quality Reporting (IQR) Program is a pay-for-reporting program for acute care hospitals.
If hospitals fail to meet the CMS Inpatient Quality Reporting (IQR) requirements will incur a penalty of 25% to their Market Basket Update (MBU). This applies to reimbursement for all Medicare claims in a given year and compounds over time.
2025 IQR Penalty Example
- Your hospital has $110MM in annual Medicare claims revenue
- You do not complete all of the IQR requirements
- The 2025 MBU is 3.4% (not including productivity adjustment of -0.5%)
- 25% penalty would result in a 2.05% payment increase versus a 2.9% payment increase
- Compounded over 3 years, the resultant financial loss would be ~2.9MM
3-YR Impact of NOT Meeting the IQR Requirements in a Single Year